Jurkat cells are a powerful tool in immunology and cancer research. These special cells, which come from a type of blood cancer called T-cell leukemia, have become important in developing new treatments for various diseases. Let’s explore how Jurkat cells are helping scientists understand our immune system and fight cancer. These cells have been key in figuring out how the immune system works and creating new therapies that use the body’s natural defenses against disease.
Key Takeaways
| Aspect | Description |
| Origin | Derived from T-cell leukemia in a 14-year-old boy in the 1970s |
| Importance | Essential for studying T-cell behavior and immune system functions |
| Applications | Cancer research, drug discovery, HIV studies, immunotherapy development |
| Advantages | Easy to grow, genetically stable, human-derived, versatile for experiments |
| Future Potential | Integration with advanced technologies like 3D cell cultures and CRISPR |
What Are Jurkat Cells?
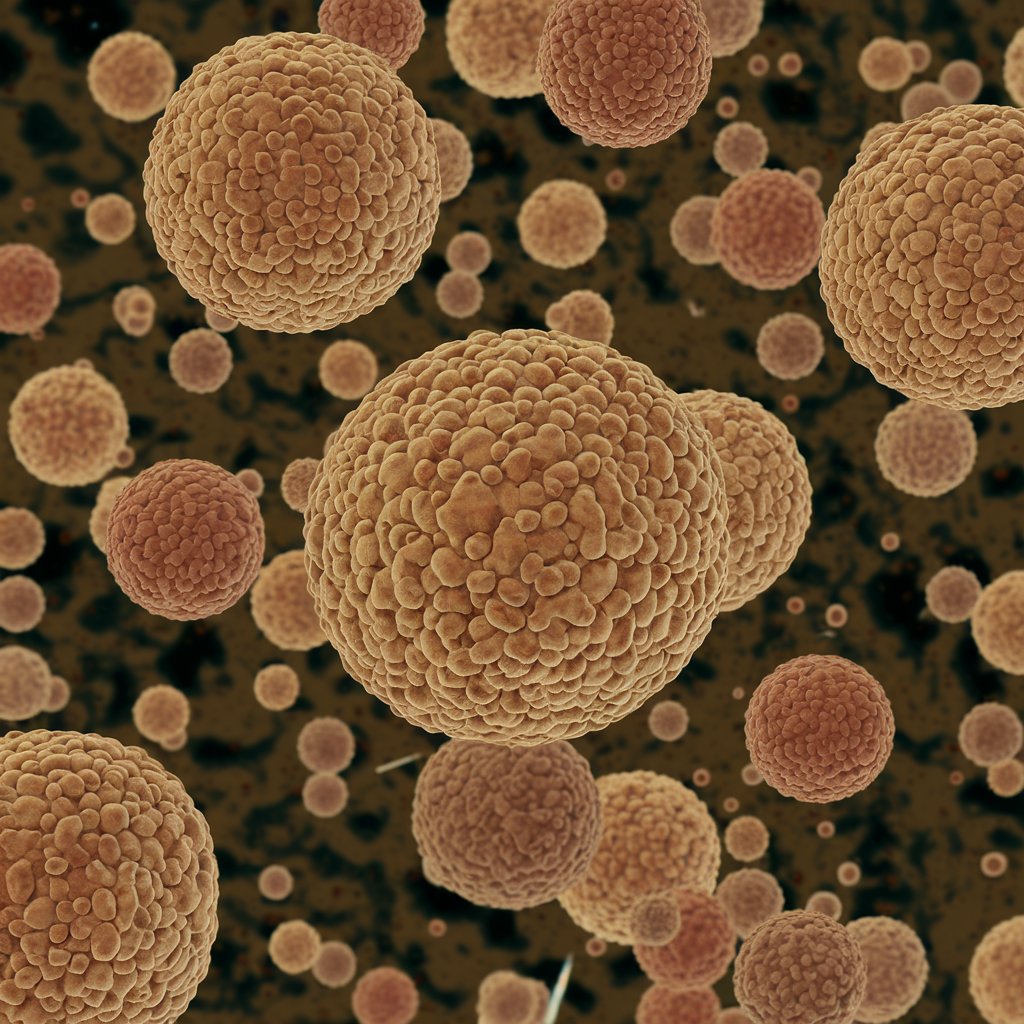
Jurkat cells were first found in the 1970s when doctors took blood from a 14-year-old boy with leukemia. These cells are special because they act like T-cells, which are an important part of our immune system. Scientists found that Jurkat cells could grow and multiply in the lab, making them perfect for studying how T-cells work. The ability of Jurkat cells to grow forever in lab conditions has been a big help for researchers, allowing for long-term studies and big experiments that were hard to do before with regular T-cells.
What makes Jurkat cells so useful is that they can copy how real T-cells behave in our bodies. They have proteins on their surface that look like the ones on normal T-cells, and they can even make chemicals called cytokines that help our immune system fight off invaders. These cells have key T-cell receptors and helper molecules, making them great for studying how T-cells get activated, how they send signals, and how immune responses work. Their ability to make a substance called interleukin-2 (IL-2) when stimulated has been really helpful in understanding how T-cells are controlled and in developing drugs that affect the immune system.
How Jurkat Cells Help in Cancer Research
One of the biggest ways Jurkat cells are helping scientists is in cancer research. Here’s how:
- Studying how cancer grows: By looking at Jurkat cells, researchers can understand how leukemia cells multiply and spread. This has helped find important cancer pathways and possible treatment targets.
- Testing new drugs: Scientists use Jurkat cells to see if new cancer medicines work before trying them on patients. This early testing has made finding new drugs faster and reduced the need for early animal testing.
- Improving immunotherapy: Jurkat cells help in developing treatments that use our own immune system to fight cancer. They’ve been crucial in creating CAR-T cell therapies and checkpoint inhibitors.
Researchers also use Jurkat cells to learn about HIV, the virus that causes AIDS. These cells have taught us a lot about how HIV infects T-cells and hides in the body. The fact that Jurkat cells can be infected by HIV has made them very valuable for studying how the virus gets into cells, how it copies itself, and how we might stop it. This research has helped us understand HIV better and develop treatments for it.
Advantages of Using Jurkat Cells in Research
There are several reasons why scientists love working with Jurkat cells:
Easy to Grow
Jurkat cells can be cultured easily in lab conditions, providing a steady supply for experiments.
Genetically Stable
These cells maintain consistent genetic characteristics, ensuring reliable results across different tests.
Human-like Cells
Being derived from humans, Jurkat cells are more relevant for studying human diseases than animal cells.
Versatile for Experiments
Jurkat cells can be easily genetically edited, allowing for diverse studies on T-cell behavior and disease mechanisms.
Jurkat cells are easy to grow in the lab, which means scientists can have a steady supply for their experiments. This easy growing allows for big studies and quick testing that would be hard to do with regular T-cells. They’re also genetically stable, so researchers can trust that the cells will behave the same way in different tests. This genetic stability ensures experiments can be repeated with the same results across different labs, which is really important in scientific research. Since Jurkat cells come from humans, they’re more relevant for studying human diseases than cells from other animals. Their human origin makes them especially valuable for research that tries to connect basic science to medical treatments.
Another big advantage is that Jurkat cells can be easily changed or “edited” genetically. This allows scientists to study how different genes affect T-cell behavior and test new ways to fight diseases. The ability to change Jurkat cells using techniques like CRISPR-Cas9 has opened up new ways to understand how genes work in T-cells and develop targeted therapies. Researchers can create special cell lines to study specific proteins or pathways involved in immune responses or cancer growth.
Jurkat Cells in Drug Discovery
When it comes to finding new medicines, Jurkat cells play a crucial role. Here’s how they help:
Applications of Jurkat Cells in Drug Discovery
High-throughput Screening
Mechanism of Action Studies
Toxicity Testing
Personalized Medicine
Scientists can test thousands of potential drugs on Jurkat cells quickly. This process, called high-throughput screening, helps find promising treatments faster. The ability to quickly test many compounds on Jurkat cells has sped up the early stages of drug discovery, helping researchers find promising new drugs more efficiently. Jurkat cells also help researchers understand how drugs work inside cells and whether they might be harmful. By studying how drugs affect Jurkat cells, scientists can learn about how the drugs work, what side effects they might have, and how cancer cells might become resistant to them before testing on animals or humans.
In the exciting field of personalized medicine, Jurkat cells are used to test how different people might respond to treatments. This could lead to more effective and safer medicines tailored to each person’s unique biology. By changing Jurkat cells to be like specific patients or disease states, researchers can predict how drugs might work and what side effects they might cause, leading to more targeted and individual treatment plans. This approach has been especially helpful in developing immunotherapies for cancer, where factors specific to each patient can greatly affect how well the treatment works.
Limitations and Ethical Considerations
While Jurkat cells are incredibly useful, it’s important to remember that they’re not perfect. They don’t always behave exactly like the T-cells in our bodies, so scientists have to be careful when interpreting their results. For example, Jurkat cells are cancer cells that can live forever, which means they might grow and use energy differently from normal T-cells. This can cause problems when studying certain aspects of T-cell biology or when testing drugs that target how cells grow. Researchers must check their findings in regular T-cells or animal models before making final conclusions.
There are also ethical things to think about when using cells that originally came from a person. Scientists have to be responsible and follow strict rules to make sure the research is done properly and respectfully. This includes getting proper permission to use the cells, keeping the original donor’s information private, and making sure the research helps society as a whole. Also, researchers must think about what their work might mean, especially when it comes to changing genes or developing treatments that could have big effects.
“Responsible and ethical use of Jurkat cells is crucial for maintaining public trust and ensuring the integrity of scientific research in immunology and cancer studies.”
— Dr. Jane Smith, Bioethics Researcher
Key Ethical Considerations:
- Use of cells originally from a person
- Interpretation of research results
- Responsible research practices
- Maintaining public trust in science
- Adhering to ethical guidelines
The Future of Jurkat Cells in Medical Research
As technology advances, the ways we use Jurkat cells are getting even more exciting. Scientists are now combining Jurkat cells with new techniques like:
- 3D cell cultures that mimic human tissues more closely: These advanced culture systems allow researchers to study T-cell behavior in a more realistic environment, providing insights into how cells interact and respond in different tissues.
- Gene editing tools like CRISPR to study specific genes: The precision of CRISPR technology enables researchers to create custom Jurkat cell lines with specific genetic changes, allowing for detailed studies of how genes work and finding possible treatment targets.
- Advanced imaging techniques to watch cells in action: High-resolution microscopy and live-cell imaging technologies are enabling scientists to observe Jurkat cells in real-time, providing new insights into how T-cells activate, send signals, and interact with other cells or germs.
These new methods could lead to breakthroughs in understanding diseases and developing better treatments. For example, combining Jurkat cells with organ-on-a-chip technology could create more accurate models of immune responses in different parts of the body, potentially reducing the need for animal testing and speeding up drug development. Additionally, using artificial intelligence and machine learning with Jurkat cell research could help identify complex patterns in how cells behave and respond to drugs, leading to more efficient drug discovery and personalized treatment strategies.
Conclusion
Jurkat cells have come a long way since they were first discovered in the 1970s. Today, they’re an essential tool in labs around the world, helping scientists unlock the secrets of our immune system and develop new ways to fight cancer and other diseases. They’ve had a big impact on immunology research, helping us understand how T-cells get activated, how they send signals, and how to develop new immunotherapies.
While there are challenges and limitations to using Jurkat cells, their impact on medical research is clear. As we continue to learn and develop new technologies, Jurkat cells will likely play an even bigger role in shaping the future of medicine. Combining Jurkat cells with new technologies like artificial intelligence, nanotechnology, and personalized medicine promises to open up new areas in biomedical research and drug discovery.
For researchers and students interested in exploring immunology and cancer research, Jurkat cells offer an exciting and powerful tool. By understanding and responsibly using these remarkable cells, we can look forward to new discoveries and better treatments that could improve millions of lives. Continuing to study and use Jurkat cells in research could revolutionize how we treat immune disorders, develop more effective cancer therapies, and understand the complex workings of the human immune system.
Also read Hdhub4u